Emergency and critical care
 Emergency and critical care are specialized branches of medicine focused on providing immediate and life-saving interventions to patients with acute, life-threatening illnesses or injuries. These fields demand rapid assessment, decisive action, and advanced medical expertise to stabilize patients and prevent further deterioration.
Emergency and critical care are specialized branches of medicine focused on providing immediate and life-saving interventions to patients with acute, life-threatening illnesses or injuries. These fields demand rapid assessment, decisive action, and advanced medical expertise to stabilize patients and prevent further deterioration.
Emergency Care:
Emergency care encompasses the initial assessment, stabilization, and treatment of patients presenting with urgent medical needs. It operates within emergency departments (EDs) and pre-hospital settings (e.g., ambulances, helicopters).
- Key Aspects:
- Rapid Triage: Prioritizing patients based on the severity of their condition.
- Initial Resuscitation: Addressing immediate life threats, such as airway obstruction, breathing difficulties, and circulatory collapse.
- Stabilization: Providing interventions to stabilize vital signs and prevent further deterioration.
- Diagnostic Evaluation: Performing necessary tests to determine the underlying cause of the patient’s condition.
- Emergency Treatment: Administering medications, performing procedures, and providing supportive care.
- Transfer: Arranging for transfer to a critical care unit or other appropriate facility when needed.
- Common Emergency Conditions:
- Cardiac arrest
- Stroke
- Trauma (e.g., motor vehicle accidents, falls)
- Severe respiratory distress
- Sepsis
- Acute poisoning
- Severe allergic reactions (anaphylaxis)
- Acute abdominal emergencies
Critical Care:
Critical care, also known as intensive care, involves the specialized management of critically ill patients in intensive care units (ICUs). These units are equipped with advanced monitoring and life support systems.
- Key Aspects:
- Advanced Monitoring: Continuous monitoring of vital signs, including heart rate, blood pressure, oxygen saturation, and respiratory function.
- Life Support: Providing interventions such as mechanical ventilation, vasopressor support, and renal replacement therapy.
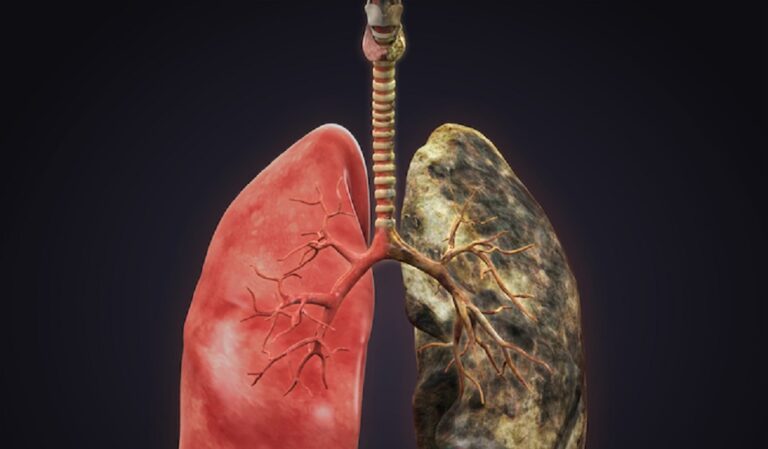
- Organ System Support: Managing organ dysfunction, such as acute respiratory failure, acute kidney injury, and circulatory shock.
- Invasive Procedures: Performing procedures such as central line insertion, arterial line placement, and endotracheal intubation.
- Multidisciplinary Care: Collaboration among physicians, nurses, respiratory therapists, and other healthcare professionals.
- Pharmacological Management: Administering complex medication regimens.
- Nutritional Support: Providing specialized nutritional support to critically ill patients.
- Common Critical Care Conditions:
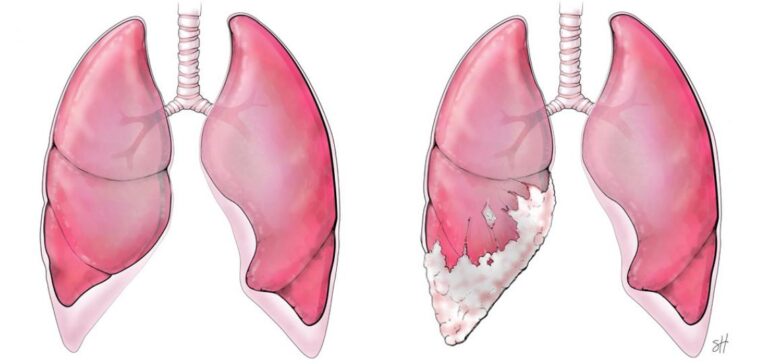
- Acute respiratory distress syndrome (ARDS)
- Sepsis and septic shock
- Multiple organ dysfunction syndrome (MODS)
- Severe trauma
- Post-cardiac arrest care
- Neurological critical care (e.g., stroke, traumatic brain injury)
- Post-surgical critical care
Differences Between Emergency and Critical Care:
- Setting: Emergency care occurs primarily in EDs and pre-hospital settings, while critical care occurs in ICUs.
- Duration of Care: Emergency care is typically short-term, focusing on initial stabilization, while critical care involves prolonged management of critically ill patients.
- Intensity of Care: Critical care involves a higher level of monitoring, life support, and invasive procedures compared to emergency care.
- Focus: Emergency care focuses on immediate stabilization and treatment of life-threatening conditions, while critical care focuses on managing organ dysfunction and preventing further deterioration.
Key Components of Both Fields:
- Rapid Assessment: The ability to quickly assess a patient’s condition and identify life-threatening problems.
- Effective Communication: Clear and concise communication among healthcare professionals and with patients and their families.
- Teamwork: Collaboration among healthcare professionals to provide coordinated care.
- Evidence-Based Practice: Using the best available evidence to guide clinical decision-making.
- Ethical Considerations: Addressing ethical dilemmas related to end-of-life care and resource allocation.
Technological Advances:
Both emergency and critical care benefit from technological advancements, including:
- Advanced monitoring devices
- Mechanical ventilators
- Extracorporeal membrane oxygenation (ECMO)
- Point-of-care ultrasound
- Electronic health records
Challenges:
- Resource limitations, especially in low-resource settings.
- Increasing patient acuity and complexity.
- Staffing shortages.
- Burnout among healthcare professionals.
- Ethical dilemmas related to resource allocation and end-of-life care.
Emergency and critical care are essential components of modern healthcare, providing life-saving interventions to patients with the most severe illnesses and injuries. Continuous improvement in training, technology, and systems of care is crucial for optimizing patient outcomes.
Other Posts