Testicular Cancer
Testicular Cancer: A Comprehensive Guide to the Young Man’s Cancer
Introduction: A Curable Crisis
Testicular cancer, while relatively rare (about 1% of male cancers), holds a unique and critical position in oncology. It is the most common solid tumor in men aged 15-35, striking at the prime of life. Yet, it is also one of the most curable cancers, with an overall survival rate exceeding 95%. This high cure rate is a triumph of modern medicine, but it hinges on one non-negotiable factor: early detection and prompt treatment. The journey from a suspicious lump to cure is typically short but intense, involving specialized surgery, potential chemotherapy, and a strong focus on preserving fertility and long-term health. This guide provides a detailed, evidence-based overview of testicular cancer, from its first signs to life after cure.
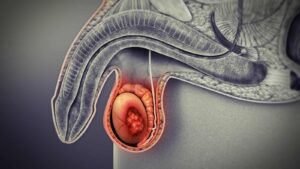
Part 1: Understanding the Testicle and Types of Tumors
The testicles (testes) are male sex glands responsible for producing sperm and testosterone. Most testicular cancers originate in the germ cells—the cells that make sperm. These are categorized into two main types, which guide treatment:
1. Seminomas (40-45% of cases):
Typical Age: Men in their 30s and 40s.
Characteristics: Tend to grow and spread more slowly. Are highly sensitive to radiation therapy and chemotherapy.
Subtypes: Classic seminoma and spermatocytic seminoma (rarer, in older men).
2. Non-Seminomas (55-60% of cases):
Typical Age: Men in their late teens, 20s, and early 30s.
Characteristics: Often grow and spread more rapidly. Comprise a mix of different cell types (embryonal carcinoma, yolk sac tumor, choriocarcinoma, teratoma). Treatment is primarily chemotherapy and surgery.
Mixed Germ Cell Tumors: Many tumors contain both seminoma and non-seminoma elements and are treated as non-seminomas.
Other Rare Types: Leydig cell tumors, Sertoli cell tumors (stromal tumors), and lymphoma (in older men).
Part 2: Risk Factors and the Role of Cryptorchidism
The exact cause is unknown, but several key risk factors are established:
Cryptorchidism (Undescended Testicle): The strongest risk factor. A testicle that fails to move down into the scrotum before birth carries a risk 3-15 times higher. Even if surgically corrected (orchiopexy), the risk remains elevated, and it affects both testicles.
Family History: Having a father or brother with testicular cancer increases risk.
Personal History: A man with cancer in one testicle has a 1-2% lifetime risk of developing it in the other.
Age: Peak incidence is ages 20-34.
Race/Ethnicity: More common in white men than in Black, Asian, or Hispanic men.
HIV/AIDS: Some evidence suggests a moderately increased risk.
NOT linked to: Vasectomy, sports injuries, or sexual activity.
Part 3: Signs, Symptoms, and the Crucial Self-Exam
Early detection is paramount. Symptoms are usually unilateral (affect one testicle).
Primary Symptoms:
A Painless Lump or Nodule: The most common sign. Often felt on the front or side of the testicle. It usually feels firm or hard.
Testicular Swelling or Enlargement: The entire testicle may feel larger, heavier, or firmer than normal.
A Change in Consistency: The testicle may feel unusually hard or develop an irregular shape.
Dull Ache or Heaviness: In the scrotum, lower abdomen, or groin. Note: Only about 20% of cases involve significant pain, which can lead to misdiagnosis as epididymitis.
Symptoms of Advanced (Metastatic) Disease:
If the cancer has spread, symptoms may include:
Lower back pain (from spread to lymph nodes).
Shortness of breath, chest pain, or cough (from lung metastases).
Swelling in one or both legs (from blocked lymph nodes).
Enlarged or tender breasts (gynecomastia) – caused by certain tumors secreting hormones (HCG).
Testicular Self-Examination (TSE):
While no major organization recommends formal monthly TSE for all men, knowing your own body is critical.
When: Perform during or after a warm shower, when scrotal skin is relaxed.
How: Gently roll each testicle between your thumb and fingers. Feel for any hard lumps, nodules, or changes in size, shape, or consistency. The epididymis (a soft, rope-like structure at the back) is normal.
Action: If you notice any change, see a doctor within two weeks. Do not wait.
Part 4: Diagnosis and Staging – The Roadmap to Cure
Diagnostic Steps:
Clinical Exam: A urologist will examine the testicles, abdomen, and lymph nodes.
Scrotal Ultrasound: The definitive diagnostic imaging test. It can confirm the presence of a solid, intratesticular mass (almost always cancer) and distinguish it from benign conditions like a hydrocele or spermatocele.
Blood Tumor Markers: Crucial for diagnosis, staging, and monitoring.
Alpha-fetoprotein (AFP): Elevated in non-seminomas only.
Beta-human chorionic gonadotropin (Beta-hCG): Elevated in some seminomas and non-seminomas.
Lactate Dehydrogenase (LDH): A non-specific marker of cell turnover; elevated in bulky disease.
A key principle: A solid mass on ultrasound + elevated tumor markers = testicular cancer. A normal marker does NOT rule out cancer (especially pure seminoma).
Radical Inguinal Orchiectomy: The primary diagnostic and therapeutic surgery. The affected testicle is removed through an incision in the groin (not the scrotum). This approach prevents spreading cancer cells. The tissue is then analyzed to confirm the type and extent of the cancer.
Staging (Determining Spread):
After orchiectomy, staging tests determine if the cancer has spread.
Stage I: Confined to the testicle.
Stage II: Spread to retroperitoneal lymph nodes (in the back of the abdomen).
Stage III: Spread to distant organs (lungs, liver, brain, bones).
Imaging for Staging: CT scans of the abdomen/pelvis and chest are standard. A brain MRI or bone scan may be done if symptoms suggest spread.
Part 5: Treatment – A Highly Tailored, Curative Approach
Treatment is based on tumor type (seminoma vs. non-seminoma), stage, and risk level. It is one of the most successful models in all of oncology.
1. Surgery:
Radical Inguinal Orchiectomy: As described above, for all cases.
Retroperitoneal Lymph Node Dissection (RPLND): A major abdominal surgery to remove lymph nodes. Used for:
Non-seminoma: As primary treatment for low-stage disease or after chemotherapy to remove residual masses.
Seminoma: Rarely, for resistant masses after chemo/radiation.
2. Active Surveillance:
For Stage I disease with favorable features. Involves close monitoring (tumor markers, exams, CT scans) to avoid unnecessary treatment, as many men are already cured by orchiectomy alone. Requires high patient compliance.
3. Radiation Therapy:
Used almost exclusively for seminomas. Effective at killing microscopic cancer cells in the abdominal lymph nodes (Stage I-IIA). Side effects include fatigue, nausea, and a small increased long-term risk of secondary cancers.
4. Chemotherapy:
The cornerstone for advanced or metastatic disease and for non-seminomas.
BEP Chemotherapy: A 3-drug combination (Bleomycin, Etoposide, Cisplatin) given in cycles. It is highly effective but carries significant side effects: fatigue, nausea, low blood counts, lung toxicity (Bleomycin), kidney toxicity, neuropathy, and infertility.
Post-Chemotherapy Surgery: To remove any residual masses (often just scar tissue or mature teratoma).
Part 6: Fertility Preservation and Survivorship
Fertility must be addressed BEFORE any treatment begins.
Sperm Banking (Cryopreservation): Strongly recommended for all men before orchiectomy, and definitely before chemotherapy or radiation. Provides insurance for future family planning.
Treatment Effects: Chemotherapy and radiation can cause temporary or permanent infertility. RPLND can cause retrograde ejaculation.
Long-Term Survivorship (Life After Cure):
Men cured of testicular cancer face specific long-term risks that require lifelong monitoring:
Secondary Malignancies: Increased risk of leukemia (from chemo) and other solid tumors (from radiation).
Cardiovascular Disease: Chemotherapy (especially cisplatin) and radiation increase the long-term risk of heart disease, high blood pressure, and high cholesterol.
Metabolic Syndrome: Higher rates of obesity, diabetes, and dyslipidemia.
Hypogonadism (Low Testosterone): Can occur if the remaining testicle doesn’t fully compensate.
Psychosocial Effects: Anxiety, depression, and “scanxiety” around follow-up visits.
Care: Requires a survivorship care plan with regular check-ups focusing on these risks.
Conclusion: A Model of Success with a Lifelong View
Testicular cancer represents a monumental achievement in cancer care. What was once a deadly diagnosis is now a model of a curable disease. This success, however, is built on a foundation of self-awareness, swift medical action, and adherence to highly effective but taxing treatments. For young men, it is a life-altering event that underscores the importance of knowing one’s own body. The journey doesn’t end with remission; it transitions into a chapter of survivorship, requiring vigilance for long-term health effects and proactive planning for fertility and wellness. With early detection and expert care, the prognosis is overwhelmingly positive, allowing survivors to look forward to a full and productive life.
Key Takeaways & Action Steps:
Know what’s normal for your body. Report any changes to a doctor promptly.
A painless testicular lump is cancer until proven otherwise. Seek a urologist’s evaluation.
Sperm banking is a critical pre-treatment step. Discuss it immediately.
Follow-up care is for life. Adhere to survivorship monitoring schedules.
Resources:
Testicular Cancer Society: www.testicularcancersociety.org
American Cancer Society: Detailed guide on testicular cancer.
The ULMAN Foundation: Support for young adult cancer patients.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. If you have concerns about your health, please consult a urologist immediately.