Cervical Cancer
 Cervical cancer, a malignancy that develops in the cells of the cervix (the lower part of the uterus that connects to the vagina), is a significant global health concern, particularly in low- and middle-income countries. Understanding the causes, risk factors, symptoms, screening methods, and treatment options is crucial for prevention and early intervention.
Cervical cancer, a malignancy that develops in the cells of the cervix (the lower part of the uterus that connects to the vagina), is a significant global health concern, particularly in low- and middle-income countries. Understanding the causes, risk factors, symptoms, screening methods, and treatment options is crucial for prevention and early intervention.
The Role of HPV:
- Human papillomavirus (HPV) is the primary cause of cervical cancer.
- HPV is a common sexually transmitted infection (STI), and most people will contract it at some point in their lives.
- While many HPV types are harmless and clear on their own, certain high-risk types can cause cellular changes that lead to cancer.
- Persistent infection with high-risk HPV types is the most significant risk factor for cervical cancer.
Risk Factors Beyond HPV:
While HPV is the main culprit, other factors can increase the risk of developing cervical cancer:
- Smoking: Smoking weakens the immune system, making it harder to fight off HPV infection.
- Weakened Immune System: Conditions like HIV/AIDS or immunosuppressant medications increase susceptibility.
- Multiple Sexual Partners: Increases the risk of HPV exposure.
- Early Age at First Sexual Intercourse: Increases the risk of HPV exposure.
- Long-Term Use of Oral Contraceptives: Some studies suggest a slightly increased risk.
- Multiple Pregnancies: May slightly increase risk.
- Family History: A family history of cervical cancer may indicate a genetic predisposition.
- Socioeconomic Factors: Limited access to healthcare and screening increases risk.
Symptoms:
In the early stages, cervical cancer often has no noticeable symptoms. As the cancer progresses, symptoms may include:
- Abnormal Vaginal Bleeding: Bleeding between periods, after intercourse, or after menopause.
- Unusual Vaginal Discharge: Watery, bloody, or foul-smelling discharge.
- Pelvic Pain: Pain during intercourse or persistent pelvic pain.
Screening and Diagnosis:
Regular screening is essential for detecting precancerous changes and early-stage cervical cancer:
- Pap Smear (Pap Test):
- This test collects cells from the cervix to check for abnormalities.
- It can detect precancerous changes, allowing for early intervention.
- This test collects cells from the cervix to check for abnormalities.
- HPV Testing:
- This test detects the presence of high-risk HPV types.
- It can be used alone or in conjunction with a Pap smear.
- This test detects the presence of high-risk HPV types.
- Colposcopy:
- If a Pap smear or HPV test shows abnormalities, a colposcopy is performed.
- This procedure uses a magnified lens to examine the cervix and take tissue samples (biopsies) for further analysis.
- If a Pap smear or HPV test shows abnormalities, a colposcopy is performed.
- Biopsy:
- A biopsy is the definitive diagnostic method, taking a small tissue sample to be examined under a microscope for cancerous cells.
- A biopsy is the definitive diagnostic method, taking a small tissue sample to be examined under a microscope for cancerous cells.
Treatment Options:
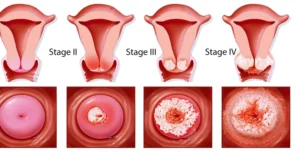
Treatment for cervical cancer depends on the stage of the cancer:
- Precancerous Changes (Cervical Intraepithelial Neoplasia or CIN):
- Cryosurgery (freezing).
- Laser ablation (using a laser to destroy abnormal tissue).
- Loop electrosurgical excision procedure (LEEP) (using an electrical wire loop to remove abnormal tissue).
- Conization (removing a cone-shaped piece of cervical tissue).
- Cryosurgery (freezing).
- Early-Stage Cervical Cancer:
- Radical hysterectomy (removal of the uterus and cervix).
- Radiation therapy.
- Chemotherapy, often combined with radiation.
- Radical hysterectomy (removal of the uterus and cervix).
- Advanced Cervical Cancer:
- Radiation therapy, often combined with chemotherapy.
- Targeted therapy.
- Palliative care to manage symptoms and improve quality of life.
- Radiation therapy, often combined with chemotherapy.
Prevention:
- HPV Vaccination:
- The HPV vaccine protects against the high-risk HPV types that cause most cervical cancers.
- It is most effective when given before sexual activity begins.
- The HPV vaccine protects against the high-risk HPV types that cause most cervical cancers.
- Regular Screening:
- Following recommended screening guidelines is crucial for early detection.
- Safe Sex Practices:
- Using condoms can reduce the risk of HPV transmission.
- Using condoms can reduce the risk of HPV transmission.
- Smoking Cessation:
- Quitting smoking reduces the risk of cervical cancer.
- Quitting smoking reduces the risk of cervical cancer.
- Healthy Lifestyle:
- Eating a healthy diet, and regular exercise can support immune system health.
- Eating a healthy diet, and regular exercise can support immune system health.
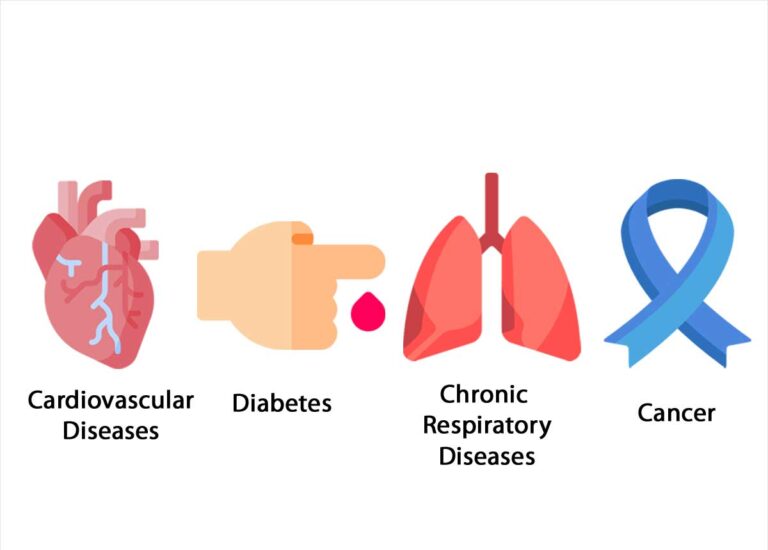
Global Impact and Disparities:
Cervical cancer disproportionately affects women in low- and middle-income countries due to limited access to screening and vaccination. Addressing these disparities requires:
- Increased access to HPV vaccination.
- Improved screening programs.
- Affordable and accessible treatment.
- Public health education campaigns.
Cervical cancer is largely preventable, and early detection significantly improves outcomes. By promoting HPV vaccination, regular screening, and healthy lifestyle choices, we can reduce the burden of this disease and save lives.
Other Posts