Colon Cancer
Colon Cancer: A Comprehensive Guide to Prevention, Detection, and Treatment
Introduction: The Preventable Cancer
Colon (colorectal) cancer is a formidable adversary, ranking as the second leading cause of cancer death in the United States when men and women are combined. Yet, it holds a unique and powerful distinction: it is one of the most preventable and, when caught early, most curable major cancers. This duality defines the modern approach to colon cancer: a disease that can largely be stopped before it starts through screening, yet one that remains deadly when allowed to progress silently. The journey from the first abnormal cell to invasive cancer is slow, taking 10 to 15 years on average, providing a critical window of opportunity. This guide details the biology of colon cancer, the transformative power of screening, the latest treatment paradigms, and the proactive lifestyle strategies that can significantly reduce individual risk.
Part 1: Understanding the Anatomy and the Adenoma-Carcinoma Sequence
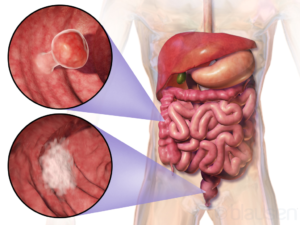
Colon cancer almost always begins as a polyp, a small, benign clump of cells on the inner lining of the colon or rectum.
Anatomy: The colon (large intestine) is the final 5-6 feet of the digestive tract, responsible for absorbing water and electrolytes and forming stool. The rectum is the last 6 inches.
The Adenoma-Carcinoma Sequence: This is the stepwise process by which most colon cancers develop:
Normal Mucosa: Healthy lining of the colon.
Aberrant Crypt Foci: The earliest microscopic change.
Adenomatous Polyp (Adenoma): A benign, precancerous growth. Not all polyps become cancer, but nearly all colon cancers start as adenomas.
Dysplasia: Cells within the polyp become increasingly abnormal.
Invasive Adenocarcinoma: Cancer cells break through the inner wall (mucosa) and invade deeper layers, gaining the potential to spread.
Key Takeaway: Removing polyps during colonoscopy interrupts this sequence and prevents cancer.
Part 2: Risk Factors: Non-Modifiable and Modifiable
Understanding risk guides screening intensity and prevention efforts.
Non-Modifiable Factors:
Age: Risk increases sharply after 45. 90% of cases are diagnosed in those 50+.
Personal History: A personal history of adenomatous polyps or inflammatory bowel disease (Ulcerative Colitis, Crohn’s Colitis).
Family History: A first-degree relative (parent, sibling, child) with colon cancer or advanced polyps, especially if diagnosed before 50.
Inherited Syndromes (5-10% of cases):
Lynch Syndrome (Hereditary Non-Polyposis Colorectal Cancer – HNPCC): The most common inherited cause. Carries a very high lifetime risk.
Familial Adenomatous Polyposis (FAP): Causes hundreds to thousands of polyps, with a near 100% risk of cancer by age 40 if untreated.
Race/Ethnicity: African Americans have the highest incidence and mortality rates in the U.S.
Modifiable Risk Factors (Lifestyle-Associated):
Diet: A diet high in red meat (beef, pork, lamb) and processed meats (bacon, sausage, deli meats) and low in fruits, vegetables, and whole grains.
Physical Inactivity.
Obesity, particularly carrying excess fat around the waist.
Smoking.
Heavy Alcohol Use (more than 2 drinks per day for men, 1 for women).
Part 3: Symptoms and Signs – Listening to Your Body
Early-stage colon cancer often has no symptoms. When symptoms appear, the cancer is often more advanced.
Warning Signs (“The Red Flags”):
A Persistent Change in Bowel Habits: Diarrhea, constipation, or narrowing of the stool that lasts more than a few days.
Rectal Bleeding or Blood in the Stool: Blood may appear bright red or make stool look dark brown or black (tarry).
Persistent Abdominal Discomfort: Cramps, gas, pain, or a feeling of being bloated or full.
A Feeling That the Bowel Doesn’t Empty Completely.
Unexplained Weakness or Fatigue.
Unintended Weight Loss.
Crucial Point: Do not assume rectal bleeding is from hemorrhoids. See a doctor for any new or persistent symptom. Hemorrhoids are common, but cancer must be ruled out.
Part 4: Screening – The Cornerstone of Prevention and Early Detection
Screening saves lives. It can find cancer early (when treatment is most effective) and, crucially, find and remove precancerous polyps.
Guidelines (for Average-Risk Adults):
Start at age 45 for all average-risk individuals. Those with a family history or other risk factors may need to start earlier.
Options are divided into two categories:
A. Tests That Can Detect Cancer and Prevent It (Structural Exams):
Colonoscopy (Gold Standard):
How: A flexible, lighted tube examines the entire colon. Polyps can be removed and biopsies taken during the procedure.
Interval: Every 10 years if normal.
Advantage: Therapeutic and diagnostic. If a high-quality prep and exam are done, it’s the most comprehensive test.
CT Colonography (“Virtual Colonoscopy”):
How: Uses CT scans to create 3D images of the colon.
Interval: Every 5 years.
Disadvantage: If polyps are found, a traditional colonoscopy is still needed to remove them.
B. Stool-Based Tests (Primarily Detect Cancer):
These are less invasive but must be done more frequently. A positive result must always be followed by a colonoscopy.
FIT (Fecal Immunochemical Test): Detects hidden blood in stool. Annual.
FIT-DNA Test (Cologuard®): Detects blood and altered DNA from cancer or polyp cells. Every 3 years.
The Best Test is the One That Gets Done. Discuss options with your doctor based on your risk and preference.
Part 5: Diagnosis and Staging – The Roadmap for Treatment
If screening or symptoms suggest cancer, a diagnostic workup begins.
Colonoscopy with Biopsy: Confirms the diagnosis. A tissue sample is analyzed by a pathologist.
Imaging for Staging: Determines the extent (stage) of the cancer.
CT Scan of Chest/Abdomen/Pelvis: To check for spread to lymph nodes, liver, or lungs.
MRI of Pelvis: Often used for rectal cancer to assess local invasion.
PET/CT Scan: Sometimes used to clarify findings from other scans.
Blood Tests: Including Carcinoembryonic Antigen (CEA), a tumor marker used to monitor treatment response and recurrence.
Staging (TNM System):
Stage 0 (Carcinoma in situ): Abnormal cells only in the inner lining.
Stage I: Cancer has grown into deeper layers of the colon wall.
Stage II: Cancer has grown through the colon wall but not to lymph nodes.
Stage III: Cancer has spread to nearby lymph nodes.
Stage IV (Metastatic): Cancer has spread to distant organs (liver, lungs, peritoneum).
Part 6: Treatment – A Multidisciplinary, Personalized Approach
Treatment depends on stage, location, and the tumor’s molecular/genetic profile.
Surgery:
Colectomy: The primary treatment for colon cancer. The cancerous segment of colon and nearby lymph nodes are removed. Minimally invasive (laparoscopic or robotic) surgery is often used for faster recovery.
Chemotherapy:
Adjuvant Chemotherapy: Given after surgery for Stage III and some high-risk Stage II cancers to kill any remaining microscopic cells.
Neoadjuvant Chemotherapy: Given before surgery for some Stage III rectal cancers and Stage IV colon cancers to shrink tumors.
Common Regimens: FOLFOX (5-FU, leucovorin, oxaliplatin), CAPEOX (capecitabine, oxaliplatin), FOLFIRI (5-FU, leucovorin, irinotecan).
Targeted Therapy & Immunotherapy:
Targeted Drugs: Attack specific molecules on cancer cells. Used for advanced/metastatic disease. Selection depends on molecular testing of the tumor:
Anti-EGFR: Cetuximab, Panitumumab (for tumors with RAS wild-type genes).
Anti-VEGF: Bevacizumab, Ramucirumab.
Immunotherapy: Uses the body’s immune system to fight cancer.
Checkpoint Inhibitors: Pembrolizumab, Nivolumab. Highly effective for the 5% of colon cancers that are microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR).
Radiation Therapy:
Used primarily for rectal cancer, often combined with chemotherapy (chemoradiation) before surgery to shrink the tumor.
Treatment of Metastatic Disease (Stage IV):
The goal is often to control the disease and prolong life. Aggressive approaches can include surgery to remove isolated liver/lung metastases combined with systemic therapy.
Part 7: Prevention and Survivorship
Lifestyle for Prevention:
Get Screened. This is #1.
Maintain a Healthy Weight.
Be Physically Active.
Eat a Diet Rich in: Whole grains, fruits, vegetables. Limit red and processed meats.
Avoid Smoking and Limit Alcohol.
Survivorship:
After treatment, survivors enter a monitoring phase with regular check-ups, CEA tests, and periodic CT scans/colonoscopies to check for recurrence. Managing long-term side effects of treatment (like neuropathy from oxaliplatin) and addressing psychosocial needs are critical components of care.
Conclusion: A Disease Defined by Opportunity
Colon cancer is a story of time. The decade-long polyp-to-cancer timeline grants us an unparalleled opportunity to intervene. Seizing this opportunity requires a two-pronged attack: population-wide adherence to screening and individual commitment to a healthy lifestyle. The medical community has provided the tools—highly effective screening tests and increasingly sophisticated treatments. The responsibility now lies with individuals and healthcare systems to ensure these tools are used. By demystifying the disease, confronting the discomfort around screening, and empowering people with knowledge, we can shift the narrative of colon cancer from a common killer to a preventable and beatable condition.
Call to Action:
If you are 45 or older (or earlier if high-risk), talk to your doctor about screening TODAY.
Know your family history.
Adopt a cancer-preventive lifestyle.
Never ignore symptoms, especially rectal bleeding.