Ovarian Cancer
Ovarian Cancer: A Comprehensive Guide to the Silent and Complex Cancer
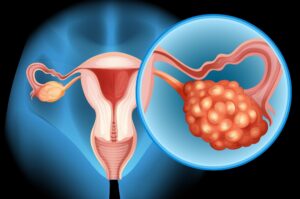
Introduction: The Elusive Adversary
Ovarian cancer remains one of the most formidable challenges in gynecologic oncology. Dubbed the “silent killer,” it is the fifth leading cause of cancer death among women and the deadliest of all gynecologic cancers. This lethality stems not from an inherent lack of treatability, but from a profound diagnostic delay. The disease typically originates deep within the pelvis, where early-stage tumors cause few or vague symptoms, leading to over 75% of cases being diagnosed at an advanced stage (III or IV). Furthermore, “ovarian cancer” is not a single disease but a collection of distinct malignancies arising from different cell types within the ovary, each with its own biology and behavior. However, the landscape is evolving with breakthroughs in genetic risk assessment, surgical precision, and the advent of maintenance therapies that are fundamentally changing the treatment paradigm. This guide provides a detailed exploration of ovarian cancer’s complexity, the quest for early detection, and the modern therapeutic strategies offering renewed hope.
Part 1: Anatomy, Types, and the Origin Debate
Recent research suggests that many of the most common and aggressive “ovarian” cancers may not originate in the ovary at all, but in the fallopian tubes.
Primary Histological Types:
Epithelial Ovarian Cancers (EOCs): ~90% of cases. Arise from the cells covering the ovary’s surface or the lining of the fallopian tube.
High-Grade Serous Carcinoma (HGSC): The most common (~70%) and aggressive subtype. The majority harbor mutations in the BRCA1/2 genes or other homologous recombination repair (HRR) genes. Strongly linked to fallopian tube origin.
Endometrioid and Clear Cell Carcinomas: Often associated with endometriosis. Tend to be diagnosed at earlier stages.
Mucinous Carcinoma: Rare; must be differentiated from metastatic cancers from the GI tract (e.g., appendix, colon).
Low-Grade Serous Carcinoma (LGSC): Less common, less responsive to chemotherapy, more indolent but persistent.
Germ Cell Tumors: ~5% of cases. Arise from egg-producing cells. Occur in younger women (teens, 20s) and are often highly curable.
Sex Cord-Stromal Tumors: ~5% of cases. Arise from hormone-producing tissues. Often present with hormonal symptoms and have a good prognosis.
Part 2: Risk Factors, Genetics, and the Paramount Role of BRCA
Non-Modifiable Factors:
Age: Risk increases with age; median diagnosis is 63.
Genetics: 10-15% of ovarian cancers are hereditary.
BRCA1 and BRCA2 Mutations: The most significant risk factor. BRCA1 carriers have a 40-60% lifetime risk; BRCA2 carriers have a 15-25% risk. These genes are involved in DNA repair; their dysfunction leads to genomic instability, particularly driving HGSC.
Lynch Syndrome (HNPCC): Increases risk for endometrioid and clear cell subtypes.
Family History: Having one first-degree relative doubles the risk; having two triples it.
Endometriosis: Increases risk for clear cell and endometrioid carcinomas.
Taller height and higher body mass index (BMI) in adulthood are associated with slightly increased risk.
Protective Factors:
Pregnancy, Breastfeeding.
Long-Term Use of Oral Contraceptives: Reduces risk by up to 50% with 5+ years of use.
Tubal Ligation or Hysterectomy.
Part 3: Signs and Symptoms – Breaking the “Silent” Myth
Ovarian cancer is not truly asymptomatic. Symptoms exist but are non-specific and easily attributed to common gastrointestinal or menstrual issues. The key is their persistence, frequency, and recent onset.
The “BE UPT” Symptom Index (Persistent & New):
Bloating or increased abdominal size.
Early satiety (feeling full quickly) or difficulty eating.
Urinary symptoms (urgency, frequency).
Pelvic or abdominal pain.
Tiredness, unexplained weight loss, changes in bowel habits.
Clinical Imperative: Symptoms that are new, persistent (occurring >12 days/month), and worsening over 4-6 weeks warrant a gynecologic evaluation, including a pelvic exam and transvaginal ultrasound.
Part 4: Diagnosis and Staging – The Surgical Imperative
There is no effective screening test for the general population (CA-125 and ultrasound have high false-positive rates). Diagnosis, therefore, often follows symptom investigation.
Clinical Evaluation: Pelvic exam may reveal a pelvic mass or ascites (fluid in the abdomen).
Imaging: Transvaginal Ultrasound (TVUS) is the primary imaging tool to characterize an ovarian mass. CT scan of the abdomen/pelvis is used for staging to assess spread.
Blood Test – CA-125: A tumor marker often elevated in epithelial ovarian cancer (especially HGSC). It is not a screening tool but is useful for monitoring treatment response and recurrence. Can be falsely elevated in benign conditions (endometriosis, fibroids, menstruation).
The Gold Standard: Surgical Staging & Diagnosis
For a suspicious mass, diagnosis and staging occur simultaneously via surgery.
Optimal Cytoreductive (Debulking) Surgery: The primary treatment goal is to remove all visible tumor. This is the single most important prognostic factor for survival. It involves a total hysterectomy, bilateral salpingo-oophorectomy, omentectomy, and lymph node dissection.
Minimally Invasive vs. Open: May start laparoscopically, but often requires a vertical laparotomy (“open” surgery) to achieve optimal cytoreduction.
Biomarker Testing: Tissue from surgery is sent for histology and critical molecular testing: HRD (Homologous Recombination Deficiency) status (including BRCA and other HRR genes) and mismatch repair (MMR) status.
Part 5: Treatment – The Modern Triad and the Rise of Maintenance Therapy
Treatment follows a standard sequence for advanced disease, with variations for early-stage or rare subtypes.
Primary Treatment for Advanced Epithelial Ovarian Cancer:
1. Surgery + Chemotherapy
Primary Debulking Surgery (PDS): As described above, followed by adjuvant chemotherapy.
Neoadjuvant Chemotherapy (NACT) + Interval Debulking Surgery: For patients where optimal surgery is not possible upfront. 3-4 cycles of chemo are given to shrink tumors, followed by surgery, then more chemo. Survival outcomes are equivalent to PDS when performed appropriately.
First-Line Chemotherapy: Carboplatin + Paclitaxel, given intravenously every 3 weeks for 6 cycles. Sometimes given in a dose-dense weekly schedule.
2. The Paradigm Shift: Maintenance Therapy
After initial chemo, patients who respond enter a maintenance phase to delay recurrence.
For HRD-Positive Tumors (including BRCA mutants): PARP Inhibitor (Olaparib, Niraparib, Rucaparib) + Bevacizumab. PARP inhibitors exploit the “synthetic lethality” in HRD tumors, preventing cancer cells from repairing DNA, causing their death.
For HRD-Negative Tumors: PARP inhibitor (Niraparib) or Bevacizumab alone.
Impact: Maintenance therapy has dramatically prolonged progression-free survival (the time until the cancer returns), often by years.
Treatment for Recurrent Disease:
Ovarian cancer is characterized by a pattern of remission and recurrence. Treatment is chosen based on the “platinum-free interval” (time since last platinum chemo ended).
Platinum-Sensitive Recurrence (>6 months): Re-treated with platinum-based chemo ± bevacizumab, followed by PARP inhibitor maintenance if not previously used.
Platinum-Resistant Recurrence (<6 months): Non-platinum chemotherapies (e.g., pegylated liposomal doxorubicin, gemcitabine, topotecan) ± bevacizumab or other targeted agents.
Treatment for Rare Subtypes:
Germ Cell & Stromal Tumors: Often cured with surgery alone or surgery + specialized chemo (BEP).
LGSC: Less chemo-sensitive; often treated with hormonal therapies (letrozole) or targeted agents (MEK inhibitors).
Part 6: Prognosis, Prevention, and the Future
Prognosis: Heavily stage-dependent. 5-year survival: ~90% for Stage I, but only ~30% for Stage III/IV. However, maintenance therapies are improving these long-term statistics.
Survivorship: Involves managing long-term side effects of treatment (neuropathy, fatigue, early menopause), monitoring for recurrence (with CA-125 and exams), and addressing “scanxiety.”
Risk Reduction & Prevention:
For High-Risk Women (BRCA carriers): Risk-Reducing Salpingo-Oophorectomy (RRSO) after childbearing is complete (recommended by ages 35-40 for BRCA1, 40-45 for BRCA2). This reduces ovarian cancer risk by ~80% and breast cancer risk by 50%.
For All Women: Long-term oral contraceptive use. Awareness of symptoms.
The Future: Focuses on earlier detection (multi-analyte blood tests, “liquid biopsies”), new targeted therapies, immunotherapy combinations, and antibody-drug conjugates.
Conclusion: From a Death Sentence to a Managed Chronic Disease
Ovarian cancer is shedding its legacy of therapeutic nihilism. While the challenge of late diagnosis persists, the treatment arsenal has undergone a revolution. The standard of care now includes not just surgery and chemotherapy, but proactive genetic testing, personalized maintenance therapy, and a sophisticated understanding of molecular subtypes. For patients, this means advocating for symptom awareness, seeking care at high-volume gynecologic oncology centers specializing in complex surgery, and ensuring comprehensive tumor testing. The path forward is one of increasing personalization, where treatments are tailored to the genetic vulnerabilities of each tumor, transforming ovarian cancer from an acute crisis into a more manageable chronic condition with significantly improved quality and length of life.
Key Takeaways:
Listen to your body. Persistent, worsening abdominal/bloating symptoms need a gynecologic evaluation.
Family history matters. Discuss it with your doctor; genetic counseling may be life-saving.
Optimal initial surgery by a gynecologic oncologist is the most critical factor for survival.
Molecular testing (HRD/BRCA) of tumor tissue is mandatory to guide maintenance therapy.
PARP inhibitors have revolutionized care, keeping the cancer in remission much longer.
Resources:
National Ovarian Cancer Coalition (NOCC): www.ovarian.org
Ovarian Cancer Research Alliance (OCRA): www.ocrahope.org
American Cancer Society: Detailed guide on ovarian cancer.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. All treatment decisions must be made in consultation with a gynecologic oncologist.